by John Halamka, Life as a Healthcare CIO
The November HIT Standards Committee meeting focused on existing implementations of point to point transport standards as a foundation for its evaluation of the Direct project.
We began the meeting with a report from the Implementation Workgroup, which will gather testimony on January 10-11, 2011 about the experience of implementing standards in certified systems and achieving meaningful use goals.
We discussed the work of the other HIT Standards Committee workgroups including the upcoming effort by the Vocabulary Task Force to take testimony on device content and vocabulary standards. Given the evolving importance of home care devices, implantable devices, and mHealth, ensuring robust standards in this area is important.
We started the day's testimony noting that we will be discussing just point to point "push" use cases this month. Typical components of such an approach are a routing method, a provider directory, certificate management, auditing, and acknowledgement of delivery. Use cases covered by the "push" approach include PCP to specialist referrals, routing to registries, e-prescribing data exchanges between providers/pharmacies, and sending summaries to patients.
Here are links to the testimony:
Peter Tippett, Verizon
John Feikema, Visionshare
Joseph Carlson, Covisint
Anand Shroff, Axolotl
Cris Ross, Surescripts
Eric Dishman & Gary Binder, Intel
After the testimony we summarized the major themes.
Directories - Proposed directory options ranged from a nationally centralized yellow pages of organizations to a federated white pages of persons/departments/machines to undiscoverable local directories. Email is an example of a directory which is generally undiscoverable outside an organization. Once you know the email address of a person, email gateways route from organization to organization. Once email arrives at the organization, it is routed to the recipient using a local directory. Whatever directory and addressing scheme is chosen, it is very important that all vendors support it to achieve a network of networks that enables any provider to connect to any other provider.
Identity/Trust - Each of the vendors is using X.509 certificate-based approaches to secure organization to organization transport plus a formal certificate management approach (based on policy) to verifying identity and achieving a trust fabric. Creating a chain of trust among vendors is very important to supporting network to network transport.
Transport - SMTP/SMIME, REST, and SOAP have all been used successfully in the real world as transport standards for health information exchange. Achieving common directories and a trust fabric are more important than settling on a single transport protocol. However, in the interest of keeping the architecture simple, there should be few, not many standards options for transport. Having at least one common transport approach to enable universal addressing is desirable.
The internet itself is based on a small number of standards specifying directories such as the Domain Naming System (DNS) system, which is implemented in a federated architecture. The internet has a small set of standards enabling certificate authorities to act as "electronic notaries", establishing identity and trust. On top of this foundation of directories and trust, there are multiple transport protocols that used to support specific use cases such as HTTPS, FTP, SMTP, etc. Push-based healthcare information exchange should use an analogous approach - get the directory/addressing and identify/trust right, then use the transport standards that best support workflow and are easy to implement.
Our next steps are to get policy guidance from the HIT Policy Committee Provider Directory Workgroup, review the Implementation guides from the testifying vendors who have successfully implemented a trust fabric, and assemble a multi-stakeholder team of interested participants from the HIT Standards Committee to evaluate NHIN Direct. We'll use objective criteria, informed by today's testimony to consider NHIN Direct on its own merits, evaluating its implementation specifications against the project goals to be simple, direct, scalable, and secure transport for the little guy.
Tuesday, November 30, 2010
Healthcare Messages Over the Internet: The Direct Project
This article originally appeared in The Health Care Blog and O'Reilly Radar on Monday November 29th. Related stories include John Halamka's post on the Direct Project and the HIT Standards Committee hearing on transport standards.
by Brian Ahier, Rich Elmore and David C. Kibbe
The Direct Project announced today the completion of its open-source connectivity-enabling software and the start of a series of pilots that will be demonstrating directed secure messaging for healthcare stakeholders over the internet. The Direct Project specifies a simple, secure, scalable, standards-based way for participants to send authenticated, encrypted health information directly to known, trusted recipients over the Internet.
Also announced:

The HISP
by Brian Ahier, Rich Elmore and David C. Kibbe
The Direct Project announced today the completion of its open-source connectivity-enabling software and the start of a series of pilots that will be demonstrating directed secure messaging for healthcare stakeholders over the internet. The Direct Project specifies a simple, secure, scalable, standards-based way for participants to send authenticated, encrypted health information directly to known, trusted recipients over the Internet.
Also announced:
- A new name - the Direct Project was previously known as NHIN Direct
- An NHIN University course, The Direct Project - Where We Are Today, to be presented by Arien Malec, November 29 at 1 PM ET, sponsored by the National eHealth Collaborative
- An extensive list of HIT vendors (20+) that have announced plans to leverage the Direct Project for message transport in connection with their solutions and services
- Presentations at the HIT Standards Committee on Tuesday November 30 where three or more vendors will be announcing their support for the Direct Project.
- A thorough documentation library including a Direct Project Overview
- Best practice guidance for directed messaging based on the policy work of the Privacy and Security Tiger team
- A new web site at DirectProject.org
- A new hashtag #directproject for following the Direct Project on twitter.
What is The Direct Project?
Today, communication of health information among providers and patients is most often achieved by sending paper through the mail or via fax. The Direct Project seeks to benefit patients and providers by improving the transport of health information, making it faster, more secure, and less expensive. The Direct Project will facilitate “direct” communication patterns with an eye toward approaching more advanced levels of interoperability than simple paper can provide.
The Direct Project provides for universal boundaryless addressing to other Direct Project participants using a health internet “email-like” address.
The Direct Project focuses on the technical standards and services necessary to securely transport content from point A to point B and does not specify the actual content exchanged. When The Direct Project is used by providers to transport and share qualifying clinical content, the combination of content and The Direct Project-specified transport standards may satisfy some Stage 1 Meaningful Use requirements. For example, a primary care physician who is referring a patient to a specialist can use The Direct Project to send a clinical summary of that patient to the specialist and to receive a summary of the consultation.
How might the Direct Project be Used?
2009-10 Congress and agencies of the federal government have created regulations that require physicians and hospitals participating in the ARRA/HITECH incentives awarded for meaningful use of EHR technology to:
- send messages and data to each other for referral and care coordination purposes;
- send alerts and reminders for preventive care to their patients;
- send patients clinical summaries of their visit and of their health information
- receive lab results from labs
- send immunization and syndromic surveillance data to public health agencies
- integrate with HIT vendor systems
Each capability can be enabled with point-to-point secure e-mail or in a more integrated manner as HIT vendors and public health agencies enable communication with the Direct Project.
How will the Direct Project affect states and Health Information Exchanges?
States that are receiving federal funding to enable message exchange are being asked by the ONC to facilitate Stage 1 Meaningful Use information exchange. The Direct Project may serve as a key enabler of directed messaging for all states and Health Information Exchanges. Even states that have some level of health information exchange capability need to address areas that are currently uncovered by a regional or local Health Information Organization (HIO).
As state plans seek to address a means to fill the gaps in exchange capability coverage, the Direct Project may provide a bridge to enabling the basic exchange requirements for Stage 1 Meaningful Use. The Direct Project does not obviate the need for state planning for HIE, neither does it undercut the business case for HIOs. More robust services can be layered over simple directed messaging that will provide value to exchange participants.
There are already organizations that have announced the establishment of national clinical exchange networks, including integration with the Direct Project. States and HIO’s will need to decide how best to provide Direct Project services to their constituents, whether by partnering with existing exchange networks or incorporating direct messaging into the services they provide.
The Direct Project Implementation
The Direct Project is organizing real-world pilots to demonstrate health information exchange using The Direct Project standards and services. Six pilots are ramping up including:
Rhode Island Quality Institute, Redwood MedNet and MedAllies will be sending Continuity of Care Documents to other providers for referrals and transitions of care. Visionshare will be linking to immunization registries. Carespark (Tennesee) will be linking the VA with private clinics providing health services to veterans. And Connecticut’s Medical Professional Services, an IPA, will be linking Middlesex Hospital with primary care providers.
The Reference Implementation
To help the Direct Project implementers, an open source reference implementation of the Direct Project standards and services has been developed under the guidance of the Direct Project. To ensure the broadest possible participation, the reference implementation has been implemented in two flavors: Java and .Net.
The HISP
Connectivity among providers is facilitated by Health Information Service Providers (HISP). HISP describes both a function (the management of security and transport for directed exchange) and an organizational model (an organization that performs HISP functions on behalf of the sending or receiving organization or individual).
Best Practices
The Direct Project is bound by a set of policies that have been recommended to the HIT Policy Committee (HITPC) or are being examined by the HITPC’s Privacy and Security Tiger Team for directed messaging. Within this context, the Direct Project has developed best practice guidance for secure communication of health data among health care participants who already know and trust each other. The Direct Project assumes that the Sender is responsible for several minimum requirements before sending data, including the collection of patient consent. These requirements may or may not be handled in an electronic health record, but they are handled nonetheless, even when sharing information today via paper or fax. For example, a sender may call to ask whether a fax was sent to the correct fax number and was received by the intended provider.
The following best practices provide context for the Direct Project standards and services:
- The Sender has obtained the patient’s consent to send the information to the Receiver.
- The Sender and Receiver ensure that the patient’s privacy preferences are being honored.
- The Sender of a Direct Project transmission has determined that it is clinically and legally appropriate to send the information to the Receiver.
- The Sender has determined that the Receiver’s address is correct.
- The Sender has communicated to the receiver, perhaps out-of-band, the purpose for exchanging the information.
- The Sender and Receiver do not require common or pre-negotiated patient identifiers. Similar to the exchange of fax or paper documents, there is no expectation that a received message will be automatically matched to a patient or automatically filed in an EHR.
- The communication will be performed in a secure, encrypted, and reliable way, as described in the detailed The Direct Project technical specifications.
- When the HISP is a separate entity from the sending or receiving organization, best practice guidance for the HISP has been developed for privacy, security and transparency.
What it isn’t
The Direct Project is not targeted at complex scenarios, such as an unconscious patient who is brought by ambulance to an Emergency Department. In the unconscious patient scenario, a provider in the ED must “search and discover” whether this patient has records available from any accessible clinical source. This type of broad query is not a simple and direct and therefore requires a more robust set of health information exchange tools and services that The Direct Project does not provide.
The Direct Project in Context of the Nationwide Health Information Network
The Direct Project is an integral component in a broader national strategy to have an interconnected health system through a Nationwide Health Information Network (NHIN). The NHIN is “a set of standards, services and policies that enable secure health information exchange over the Internet. The NHIN will provide a foundation for the exchange of health IT across diverse entities, within communities and across the country, helping to achieve the goals of the HITECH Act.”
The authors:
Brian Ahier is chairman of the State of Oregon’s Health Information Technology Oversight Council Technology Workgroup. Rich Elmore is Vice President, Strategic Initiatives at Allscripts. David C. Kibbe is a family physician, senior advisor to American Academy of Family Physicians and co-founder of the Clinical Groupware Collaborative.
Labels:
Direct Project,
Directed Messaging,
NHIN Direct
Tuesday, November 23, 2010
Things We Are Grateful For This Year
For three years running now, many of us bloggers have participated in what we’ve called a “blog rally” to promote Engage With Grace – a movement aimed at making sure all of us understand, communicate, and have honored our end-of-life wishes.
The rally is timed to coincide with a weekend when most of us in the United States are celebrating Thanksgiving and are with the very people with whom we should be having these unbelievably important conversations – our closest friends and family.
At the heart of Engage With Grace are five questions designed to get the conversation about end-of-life started. We have included them at the end of this post. They are not easy questions, but they are important -- and believe it or not, most people find they actually enjoy discussing their answers with loved ones. The key is having the conversation before it’s too late.
Thank you to whomever perpetuated the myth of “death panels” for putting a fine point on all the things we don’t stand for, and in the process, shining a light on the right we all have to live our lives with intent – right through to the end.
Thank you to TEDMED for letting us share our story and our vision.
And of course, thank you to everyone who has taken this topic so seriously, and to all who have done so much to spread the word, including sharing The One Slide.
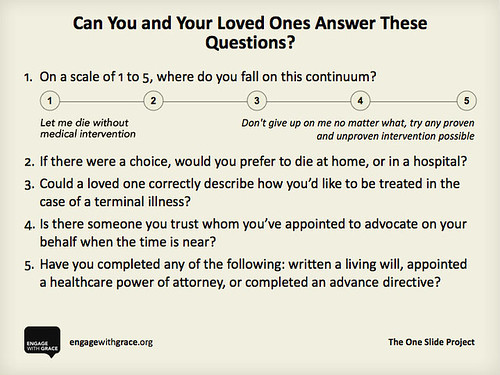
We share our thanks with you, and we ask that you share this slide with your family, friends, and followers. Know the answers for yourself, know the answers for your loved ones, and appoint an advocate who can make sure those wishes get honored – it’s something we think you’ll be thankful for when it matters most.
The rally is timed to coincide with a weekend when most of us in the United States are celebrating Thanksgiving and are with the very people with whom we should be having these unbelievably important conversations – our closest friends and family.
At the heart of Engage With Grace are five questions designed to get the conversation about end-of-life started. We have included them at the end of this post. They are not easy questions, but they are important -- and believe it or not, most people find they actually enjoy discussing their answers with loved ones. The key is having the conversation before it’s too late.
This past year has done so much to support our mission to get more and more people talking about their end-of-life wishes. We’ve heard stories with happy endings … and stories with endings that could have (and should have) been better. We have stared down political opposition. We have supported each other’s efforts. And we have helped make this a topic of national importance.
So in the spirit of the upcoming Thanksgiving weekend, we’d like to highlight some things for which we’re grateful.
Thank you to Atul Gawande for writing such a fiercely intelligent and compelling piece on “letting go”– it is a work of art, and a must read.Thank you to whomever perpetuated the myth of “death panels” for putting a fine point on all the things we don’t stand for, and in the process, shining a light on the right we all have to live our lives with intent – right through to the end.
Thank you to TEDMED for letting us share our story and our vision.
And of course, thank you to everyone who has taken this topic so seriously, and to all who have done so much to spread the word, including sharing The One Slide.
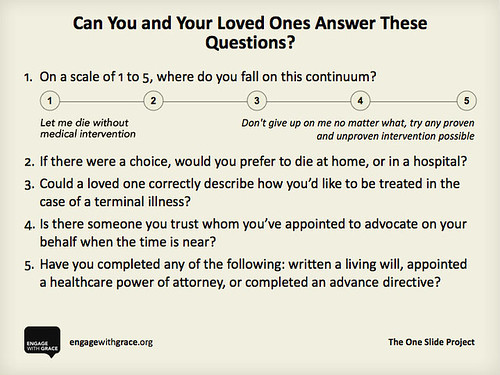
We share our thanks with you, and we ask that you share this slide with your family, friends, and followers. Know the answers for yourself, know the answers for your loved ones, and appoint an advocate who can make sure those wishes get honored – it’s something we think you’ll be thankful for when it matters most.
Here’s to a holiday filled with joy – and as we engage in conversation with the ones we love, we engage with grace.
To learn more please go to www.engagewithgrace.org. This post was written by Alexandra Drane and the Engage With Grace team. Please feel free to join our blog rally by copying this post and putting it on your own blog for this holiday weekend.
Labels:
Engage With Grace
Provider Authentication Recommendations
 Earlier this week, the HIT Policy Committee approved the recommendations of the Privacy and Security Tiger Team for provider authentication. The purpose is to support the exchange of clinical information among providers, especially in connection with meaningful use. The goal is to establish a trust framework for information exchange between the clinical systems of each provider. This is accomplished through digital credentials at an organization level, not at a person level.
Earlier this week, the HIT Policy Committee approved the recommendations of the Privacy and Security Tiger Team for provider authentication. The purpose is to support the exchange of clinical information among providers, especially in connection with meaningful use. The goal is to establish a trust framework for information exchange between the clinical systems of each provider. This is accomplished through digital credentials at an organization level, not at a person level. The Tiger Team recommended that all organizations that exchange health information should have digital certificates. This includes: "covered entities, business associates, PHR providers, public health entities, PBMs, retail pharmacies, DME suppliers, labs, imaging centers and non-providers including payers, claims clearinghouses and HIOs". The Tiger Team outlined at a high level the requirements for credentialing and the process which will involve multiple credentialing agencies nationally. It was recommended that the HIT Standards Committee establish standards for digital certificates.
EHR's should be certified based on the ability to "retrieve, validate, use, and revoke digital certificates that comply with standards". Authentication would be required for the exchange of personally identifiable health information and when the sending and/or receiving identities must be verified.
Provider Authentication Recommendations - Privacy and Security Tiger Team - 2010-11-19
Labels:
Authentication,
Healthcare Providers,
Privacy,
security,
Tiger Team
Monday, November 22, 2010
US lags in access, cost and insurance problems due to insurance design
The Commonwealth Fund study on How Health Insurance Design Affects Access to Care and Costs, by Income, in Eleven Countries found that:
- "One-third (33%) of U.S. adults went without recommended care, did not see a doctor when sick, or failed to fill prescriptions because of costs, compared with as few as 5 percent of adults in the United Kingdom and 6 percent in the Netherlands.
- One-fifth (20%) of U.S. adults had major problems paying medical bills, compared with 9 percent or less in all other countries.
- Thirty-one percent of U.S. adults reported spending a lot of time dealing with insurance paperwork, disputes, having a claim denied by their insurer, or receiving less payment than expected. Only 13 percent of adults in Switzerland, 20 percent in the Netherlands, and 23 percent in Germany—all countries with competitive insurance markets that allow consumers a choice of health plan—reported these concerns.
- The study found persistent and wide disparities by income within the U.S.—even for those with insurance coverage. Nearly half (46%) of working-age U.S. adults with below-average incomes who were insured all year went without needed care, double the rate reported by above-average-income U.S. adults with insurance.
- The U.S. lags behind many countries in access to primary care when sick. Only 57 percent of adults in the U.S. saw their doctor the same or next day when they were sick, compared with 70 percent of U.K. adults, 72 percent of Dutch adults, 78 percent of New Zealand adults, and 93 percent of Swiss adults.
- U.S. , German, and Swiss adults reported the most rapid access to specialists. Eighty percent of U.S. adults, 83 percent of German adults, and 82 percent of Swiss adults waited less than four weeks for a specialist appointment. U.K. (72%) and Dutch (70%) adults also reported prompt specialist access."
Labels:
Commonwealth Fund,
Health Insurance
Thursday, November 18, 2010
Deception On Health Care Reform
Former Corporate Communications chief for CIGNA and Humana, Wendell Potter, contends that "insurance company PR is killing health care and deceiving Americans". Potter is now the Senior Fellow on Health Care for the Center for Media and Democracy.
At a time when Republicans are planning to repeal healthcare reform, Potter argues that they "will ultimately settle for gutting the law of its provisions that protect consumers. That’s because the insurance industry is a major beneficiary of healthcare reform and they’re also a major contributor to Republican campaigns."
Two years ago, Potter quit CIGNA and testified to Congress on controversial insurance industry practices.
Here's the Democracy Now interview with Wendell Potter:
At a time when Republicans are planning to repeal healthcare reform, Potter argues that they "will ultimately settle for gutting the law of its provisions that protect consumers. That’s because the insurance industry is a major beneficiary of healthcare reform and they’re also a major contributor to Republican campaigns."
Two years ago, Potter quit CIGNA and testified to Congress on controversial insurance industry practices.
Here's the Democracy Now interview with Wendell Potter:
Labels:
CIGNA,
Health Care Reform,
Humana,
Wendell Potter
Tuesday, November 16, 2010
Fifty Nine Million
59.1 million people in the US were uninsured for at least part of the prior year.
6 times as many hypertensive and diabetic adults without health insurance last year forgo medical care.
5 times as many asthmatic adults without health insurance last year forgo medical care.
9.7 million adults with incomes 2-3 times above poverty level were uninsured for at least part of the year.
CDC estimates are based on interviews conducted during the first quarter of 2010 as part of the CDC's National Health Interview Survey (NHIS) and cover the year prior to the interview. CDC concluded:
 |
| From CDC Vital Signs - November 2010 |
"The data in this report support previous findings that continuous insurance coverage is an important factor in reducing delayed or forgone health care, which other studies have associated with avoidable hospitalizations for persons with chronic conditions. In addition, the data demonstrate that cost can be a barrier to health care, even for those with insurance coverage..."
"Like insurance coverage, family income is an important influence on receipt of health care. The data show that among persons aged 18--64 years with continuous insurance coverage, those with lower family incomes are twice as likely to forgo needed care because of cost when compared to those with higher family incomes. This disparity in health-care utilization might result from multiple factors outside the scope of this analysis, including personal choice, underinsurance, more difficulty making copayments, and barriers to accessing care (e.g., transportation costs and physician acceptance of publicly insured patients). This report focuses on persons aged 18--64 years and particularly those with chronic conditions, because these populations are large and their ability to receive all needed care has decreased substantially in recent years. As a result of near-universal coverage of persons aged ≥65 years through Medicare and expansions in coverage for persons aged ≤17 years through Medicaid and the Children's Health Insurance Program, coverage for these age groups has improved or remained relatively stable in recent years."
Labels:
CDC,
Health Insurance
Thursday, November 11, 2010
Health Wonk Review at INQRI
Check out the latest Health Wonk Review - the best of the healthcare policy blogosphere - hosted by the Interdisciplinary Nursing Quality Research Initiative (INQRI). There are some terrific posts on the mid-term elections and the implications for the Affordable Care Act.
Labels:
Health Wonk Review
Tuesday, November 9, 2010
Single Payer System Takes Center Stage in Vermont
While healthcare reform came under fire in many parts of the country, a single payer system is very much on the horizon in Vermont.
Vermont's new governor-elect Peter Shumlin makes the case for a single payer system first and foremost as an economic issue based on the trajectory of cost increases for the state, employers and individuals. Shumlin campaigned on a platform that calls for implementation of a single payer system, with benefits that follow the individual and are not a requirement of the employer. The system would reimburse based on outcomes rather than fee for service using technology for medical records and payment. It would also eliminate private insurers and their administrative costs.
 There is solid evidence to back up Shumlin's belief. Exit polls tallied 59% of Vermont voters either backing national health care reform as-is (16%) or backing expansion of reform (43%). And with the Vermont executive and legislative branches firmly controlled by one political party, there is the very real opportunity for a viable single payer system to be enacted.
There is solid evidence to back up Shumlin's belief. Exit polls tallied 59% of Vermont voters either backing national health care reform as-is (16%) or backing expansion of reform (43%). And with the Vermont executive and legislative branches firmly controlled by one political party, there is the very real opportunity for a viable single payer system to be enacted.
According to Shumlin, "in Vermont, the cost of health care is estimated to increase by $1 billion from 2010 to 2012. For the average Vermont family of four that's a $7,000 increase on top of the $32,000 that we now spend for health care coverage each year. Our rate of increase exceeds the national average. It is not sustainable. Health care costs are crippling our economy, hampering business growth, driving up property taxes, and bankrupting too many individuals. These costs must be brought under control. The only way to do this is for the state of Vermont to lead the nation in comprehensive health care reform. 47,000 Vermonters have no insurance. When these Vermonters become sick, they are faced with a choice—seek the care they need and risk bankruptcy, or avoid care and face debilitating health or even death. When they do choose to seek care, it is the insured that pay for it. This is an unacceptable choice in a civilized society. It also imposes ethical dilemmas on health care professionals trying to treat the uninsured. Unfortunately, this problem isn’t confined to the uninsured. Tens of thousands of Vermonters are underinsured. All too often Vermonters don’t get the care they need because of unaffordable deductibles, co-pays, and coinsurance."
 |
| GLENN RUSSELL, Burlington Free Press Democratic gubernatorial candidate Peter Shumlin (center) meets with Rich Elmore (left) and Maryse Laforce before speaking to employees at Allscripts in South Burlington on Tuesday, October 19, 2010. |
Earlier this year, Harvard Economics Professor William Hsiao, an expert on health care systems, was commissioned by the Vermont legislature to develop implementation plans for healthcare system options including a single payer system. In a New York Times interview, Hsiao contends that "you can have universal coverage and good quality health care while still managing to control costs. But you have to have a single-payer system to do it."
Vermont would require a waiver from the federal government to implement a single payer program. Shumlin is already lobbying President Obama about this waiver. According to Shumlin, "the waivers is the easy part. The hard part is designing a single payer health care system that works and that delivers quality health care, gets insurers off our providers' backs, has a reimbursement system that makes sense. ... I believe if we design that system, we can sell it." There is solid evidence to back up Shumlin's belief. Exit polls tallied 59% of Vermont voters either backing national health care reform as-is (16%) or backing expansion of reform (43%). And with the Vermont executive and legislative branches firmly controlled by one political party, there is the very real opportunity for a viable single payer system to be enacted.
There is solid evidence to back up Shumlin's belief. Exit polls tallied 59% of Vermont voters either backing national health care reform as-is (16%) or backing expansion of reform (43%). And with the Vermont executive and legislative branches firmly controlled by one political party, there is the very real opportunity for a viable single payer system to be enacted.According to Shumlin, "in Vermont, the cost of health care is estimated to increase by $1 billion from 2010 to 2012. For the average Vermont family of four that's a $7,000 increase on top of the $32,000 that we now spend for health care coverage each year. Our rate of increase exceeds the national average. It is not sustainable. Health care costs are crippling our economy, hampering business growth, driving up property taxes, and bankrupting too many individuals. These costs must be brought under control. The only way to do this is for the state of Vermont to lead the nation in comprehensive health care reform. 47,000 Vermonters have no insurance. When these Vermonters become sick, they are faced with a choice—seek the care they need and risk bankruptcy, or avoid care and face debilitating health or even death. When they do choose to seek care, it is the insured that pay for it. This is an unacceptable choice in a civilized society. It also imposes ethical dilemmas on health care professionals trying to treat the uninsured. Unfortunately, this problem isn’t confined to the uninsured. Tens of thousands of Vermonters are underinsured. All too often Vermonters don’t get the care they need because of unaffordable deductibles, co-pays, and coinsurance."
Labels:
Peter Shumlin,
Single Payer,
Vermont
Sunday, November 7, 2010
"Damn It, My Mom Is On Facebook" Filter
In a change of pace that will be appreciated by every parent with kids, and every kid with parents...
Labels:
Saturday Night Live
Tuesday, November 2, 2010
Being an e-patient
Dave deBronkart's speech to cancer patients at the Dana Farber / Harvard Cancer Center's Kidney Cancer Symposium.
e-Patient Dave speaking to other kidney cancer patients, June 2010 from e-Patient Dave deBronkart on Vimeo.
e-Patient Dave speaking to other kidney cancer patients, June 2010 from e-Patient Dave deBronkart on Vimeo.
Labels:
Dave deBrankart,
e-patient
Subscribe to:
Posts (Atom)









