There's one patient, one primary care physician and a couple other providers, right?
Not from the perspective of the physician who has to coordinate with 229 providers across 114 practices. A recent article in the
Annals of Internal Medicine spells out the challenge.

Dr. Mai Pham is the Senior Health Researcher and Co-Director for Quantitative Research at the Center for Studying Health System Change. She was the principal investigator for "
Primary Care Physicians' Links to Other Physicians Through Medicare Patients: The Scope of Coordination of Care".
Mai recently sat down with Healthcare Technology News to talk about the study and its implications for healthcare reform.
HTN: Please tell us about the Center for Studying Health System Change. With all the work on health care reform, what will this next year bring?
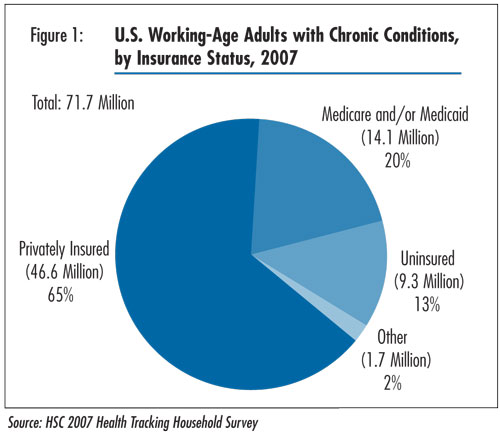
Mai Pham: HSC is a non-partisan, health policy research organization in Washington that focuses on understanding how health policy decisions affect people and health care markets. The coming months obviously will generate a lot of debate on the issues we’re interested in. I think it will be interesting to see how policymakers balance the desire to broaden insurance coverage versus the need to rein in costs and at least begin to tackle re-design of the health care delivery system.
HTN: You just completed a study which found that the typical primary care doctor may need to coordinate care with 229 doctors across 117 different practices. That’s an eye-popping statistic.
Mai Pham: It really is very daunting. We worked hard to keep our estimates on the conservative side – we focused only on Medicare patients and only physicians. If you consider younger patients and important providers like nurse practitioners, those numbers would be even larger. We imagine that a primary care doctor wouldn’t necessarily be able to name all the other doctors in his or her “peer network.”
HTN: The reality is that doctors can’t stay meaningfully in touch with this many providers, right?
Mai Pham: It is possible that physicians manage to exchange some clinical information most of the time, with the peers that they know about. But it seems far less likely either (1) that they know who all their peers are since Medicare patients can self-refer to any physician and don’t necessarily tell their primary care doctor about all their other providers; or (2) that all these physician peers can really engage in meaningful, shared decision-making, which I think is one of the tougher tasks in coordinating care.
HTN: So what happens today? And what should be happening?
Mai Pham: My guess about what’s happening today is that both patients and physicians feel overwhelmed by the fragmented nature of care and care relationships. Often it will seem to them that it’s not possible for anyone to really steer the ship in a way that is consistent with a patient’s needs and preferences. I think a more ideal situation might be one in which a patient identifies a single practice as their “medical home,” and is honest with that practice about care that they seek elsewhere. Then the medical home would have a reciprocal responsibility to choose their peers carefully based on those peers’ demonstrated willingness to communicate and coordinate with them, explain to patients why they prefer some peers to others, and not least – get paid to do that coordination work, which they don’t have under fee-for-service structures.
HTN: Since your study was limited to fee-for-service Medicare patients and didn’t consider non-physician providers, it’s likely that the actual number of provider links is greater than the median 229. Care to guess how much greater?
Mai Pham: I don’t think it would be as large as double, because Medicare patients will tend to be sicker and require more different physicians than will other patients, but I think it would be noticeably larger, especially for family practitioners who also need pediatric consultants. Let’s just say I pale at the thought….
HTN: You suggest that this fragmentation of care might be effectively addressed by formalizing relationships and tying payment to “peer webs”. Can you explain the peer web concept?
Mai Pham: Other terms that try to capture the same concept include “medical neighborhood” and “peer networks.” The concept is that no physician has sole influence over their patients’ care. Even if I am the main provider for my patient, their “medical home” if you will, I need to coordinate shared decision-making with all the other providers who also treat my patient. If you extend that one “web” for one patient to all of my core patients, you start to see the complexity of my total “peer web.” It’s really about shouldering the burden of care coordination as a primary care doctor.
HTN: You found that patients are seeing “7 different physicians from 4 different practices in a given year, and care of patients with multiple chronic illnesses is even more fragmented.” What does this fragmentation of care mean to the patient? Will peer webs help?
Mai Pham: For patients, I think it means a lot of mental energy goes into navigating the system, having potentially redundant conversations with different physicians, and in the end, not necessarily getting the care you need or want because details fall through the cracks. I think rationalizing peer webs can help, if there is an explicit understanding between different physicians and between physicians and patients that “this is what you can expect of me when you send me a referral” or “this is what we will do together when we consult you.”
HTN: What are the implications of your study on the requirements for the Advanced Medical Home?
Mai Pham: I think there is interest in broadening the medical home concept to incorporate this notion of a “medical neighborhood” in a way that sets realistic expectations for how physicians outside of the medical home will behave, and how each physician will be paid to support shared decision-making and effective coordination.
HTN: What other implications does your study have for the health care reform debate now underway?
Mai Pham: I think it is very tempting for reformers to focus on creating “winners,” for example by offering greater access to insurance coverage. The flip side of that is ensuring that once someone has insurance, they can actually get good care. Whether or not they take it as one of the early steps in reform, policymakers will eventually have to confront the need to re-design the care delivery system, or the money we spend on increasing access may not be worth it.
 Nothing like the threat of a pandemic... The Senate (finally) confirms Kathleen Sebelius for Secretary of Health and Human Services. The Wall Street Journal reports that "she was sworn in hours later and quickly went to work on the swine-flu outbreak... She'll also guide a health-care overhaul that the White House and Congress are pledging to enact this year."
Nothing like the threat of a pandemic... The Senate (finally) confirms Kathleen Sebelius for Secretary of Health and Human Services. The Wall Street Journal reports that "she was sworn in hours later and quickly went to work on the swine-flu outbreak... She'll also guide a health-care overhaul that the White House and Congress are pledging to enact this year."