Architectures
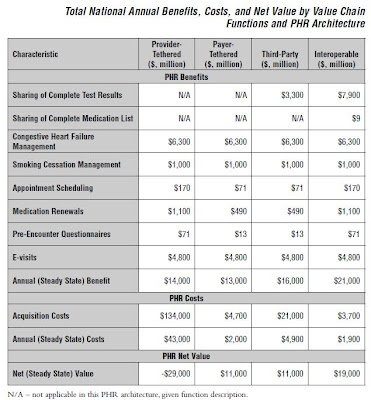
CITL's full report evaluated four different PHR architectures: 1) Provider-tethered, 2) Payer-tethered, 3) Third party and 4) Interoperable.
Tethered architectures refer to providers or payers providing the data integration to the PHR. The Third Party architecture refers to manual aggregation of health information but without the ability to integrate back to the clinical and administrative systems "in their native formats". In the Interoperable architecture, patient information flows into the PHR using standards based health information exchange from sources throughout the region and from there can be machine interpreted by the clinical and administrative systems.
The Provider-tethered architecture provides a limited view of the patient, compared to an interoperable regional approach. This architecture also requires a very large number of implementations to support 80% PHR adoption:
- Provider - 26,000
- Payer - 706
- Third Party - 3
- Interoperable - 428
The number of implementations is a major factor driving the total national installation costs.

The CITL value chain model is used to estimate the value of the PHR functions including:
1. Information Sharing
1a. Complete Test results
1b. Complete Medication lists
2. Information Self-management
2a. Congestive Heart Failure Management
2b. Smoking Cessation Management
3. Information Exchange 3a. Appointment Scheduling
3b. Medication Renewals
3c. Pre-Encounter Questionnaire
3d. e-Visits

Four of these functions contribute 95% of the value: Sharing of complete test results ($7.9); Congestive heart failure management ($6.3), e-Visits ($4.8), and Medication renewals ($1.1).
The annual steady state net value for the Interoperable architecture comes in tops at $19 billion, followed by Third-Party and Payer-tethered at $11 billion with Provider-tethered trailing at a whopping negative $29 billion.
News Analysis
So what are the strategic implications for Healthcare Organizations (HCO's)?
- HCO's won't be able to carry this on their shoulders - - the costs are prohibitive.
- HCO's will need to ensure that their clinical and administrative systems can interoperate using national standards and can participate in regional health information exchange initiatives.
- HCO's should look to collaborate and invest in PHR's that are building towards an interoperable standards-based technology platform and are able to connect with multiple providers in the region.
- HCO's will need to develop strategies which distinguish between the 1) Personal Health Record (patient-centered) and 2) the portals which connect the HCO to the patient/consumer (HCO-centered).
Many thanks to Blackford Middleton and CITL for permission to reproduce excerpts from the report.










2 comments:
Rich,
Scanned and read various sections of the new CITL report. Unfortunately, did not find as much positive things to say about the report as there were some pretty big omissions and a significantly slant/bias in the report towards clinical practices and workflow and less about consumer use/value. Also was very surprised to see complete lack of value analysis for employers, one of the major markets for PHR vendors.
While I applaud CITL for doing the study, due to a number of fatal flaws am concerned that it will hurt the market more than help it.
For a contrasting view, you can see my post last week over at www.ChilmarkResearch.com
I find it hard to get excited about the PHR concept. True, without interoperability, you don't have the ubiquity you need to even get it into the providers' hands to look at. But even if you could, the whole premise fails the WIIFM test (What's In It For Me). The key player at the table is the patient with one or more chronic conditions, who likely sees five or more clinicians over the course of the year. Even if you could get those five docs to agree on a standard and to agree (despite the risk, expense and effort) to consider what was in the record to be worthwhile, why would a patient want to share their vitals with a system engineered to discriminate against them for such disclosures. The pre-requisite for PHRs is not methodology or technology -- it's universal healthcare. Patients cannot be expected to share their information with a system that has proved itself so unworthy of their trust.
Post a Comment