Dr. Ann O'Malley and a research team from the Center for Studying Health System Change were profiled asking how care coordination could be improved through health IT. In Part II of this report, HTN sits down with Dr. O'Malley to ask about the study and its implications.
Dr. Ann O'Malley and a research team from the Center for Studying Health System Change were profiled asking how care coordination could be improved through health IT. In Part II of this report, HTN sits down with Dr. O'Malley to ask about the study and its implications.The study, published in The Journal of General Internal Medicine article, titled "Are Electronic Medical Records Helpful for Care Coordination? Experiences of Physician Practices," interviews physicians and staff with at least two years of experience with commercial ambulatory EMRs in place, along with CMO's from Health IT vendors and national thought leaders on health IT.
HTN: Why is coordination of care so difficult?
Ann O'Malley: First, it is not compensated. So coordination activities carried out by clinicians and their staff are done at the expense of other billable activities. Next, the average Medicare beneficiary sees 7 different physicians in a given year, that's a lot of people with whom that person's regular doctor may need to communicate. Third, systems are not in place to facilitate communication among clinicians caring for the same patient.
HTN: What are the primary policy and technical changes that could help?
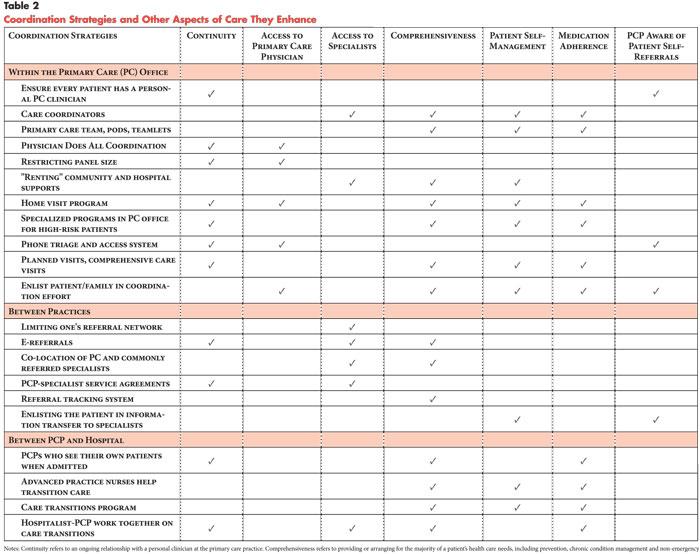
Ann O'Malley: First, the creation of incentives for providers to coordinate care and to communicate with one another would be helpful. This includes not just financial incentives, but breaking down some of the existing systematic barriers to coordination that are present in the fee-for-service system. Next, improving the basic care processes around coordination and the infrastructure to support those processes, such as improved health information technology capabilities important to coordination tasks, could be quite helpful.
HTN: You identified many opportunities to take advantage of current technology. Which of these were likely to have the biggest impact on care coordination?
Ann O'Malley: Interoperability between EMRs is key so that clinicians in different offices or across inpatient and outpatient settings can exchange patient data in a secure way that promotes coordination.
HTN: You also identified areas for EMR improvement. Which of these were likely to have the biggest impact on care coordination?
Ann O'Malley: It's hard to say at this point in HIT development. But among the clinicians we spoke with, the exchange of medication lists, problem lists, and communication around referrals and consultations as well as shared care plans were quite important.
HTN: ONC has published the rules by which eligible professionals will be receive incentive payments to be meaningful users of a certified EHR. Where are these rules on the mark, and where do they fall short in terms of facilitating coordination of care?
Ann O'Malley: They are appropriately taking an incremental approach because there is such variation in terms of EMR implementation among U.S. practitioners.
HTN: You interviewed clinicians and leaders that are working every day with EMR technology. What's their general "temperature" related to the state of Health IT and EMR's?
Ann O'Malley: In general, most clinicians would not go back to paper. They felt EMRs were an improvement for care provided within their office. For those outside of integrated delivery systems however, EMRS were not felt to be helpful as they currently are designed and used for coordination of care across offices or settings.
_____________________________
Ann S. O'Malley MD, MPH is a senior health researcher with the Center for Studying Health System Change. She conducts quantitative and qualitative research on a wide range of topics related to quality and access. She is particularly interested in primary care delivery, its intersection with specialty care, and the coordination of care from both the patient and provider perspectives. O'Malley completed her pediatrics internship at Georgetown University Medical Center and a residency in preventive medicine at the University of Maryland Medical Center. She received her master's degree in public health from Johns Hopkins and then completed a National Research Service Award fellowship in primary care research. She is board certified in preventive medicine and is a fellow of the American College of Preventive Medicine.