Thursday, March 26, 2009
The Week in Review - March 26, 2009
________________
"The number of medically disenfranchised has reached 60 million" according to a report from the National Association of Community Health Centers.
David Blumenthal, the new National Coordinator for Health Information Technology, weighs in on stimulating the adoption of health information technology. John Glaser will join David Blumenthal as an ONC advisor for 6 months, while retaining his role at Partners Healthcare.
Dr. Ashish Jha talks about the conversion to electronic medical records in this NPR interview. He found that "comprehensive" EHR systems are used by only 1.5% of hospitals and only 7.6% of hospitals have a "basic" EHR.
The California HealthCare Foundation releases a report on patient registration kiosks delivering value and increased patient satisfaction. Yet they are adopted by less than 10% of healthcare organizations.
Drs. Bates, Halamka and Middleton make the case for the effectiveness of healthcare technology.
Will IT Save Healthcare? on National Public Radio's "To the Point".
Can technology enable patients to be better advocates for their own care? The Wall Street Journal reports on how patients use "information therapy".
CCHIT plans to accelerate advanced technology certification programs in Clinical Decision Support, Interoperability, Quality and Security in order to better align with the objectives in the ARRA stimulus package.
Monday, January 5, 2009
Good Enough? The Debate Over Investments in Healthcare Technology

Are today's healthcare IT systems "good enough"?
David Blumenthal (Harvard Medical School and Institute for Health Policy) said "the debate over whether existing technology is good enough has only emerged recently, with the prospect of a huge national investment in electronic health records. What seems to be happening ... is that passionate health technology advocates fear the country could get locked into an imperfect system."
Healthcare technology interoperability is considered a key component to reduction of administrative costs and improved coordination and continuity of care. Mike Leavitt, Secretary of HHS, contends that "we're already on the road to a system that is universally accessible and secure. Health information experts ... have been working on foundational health IT standards and have made substantial progress."
In Next Steps for Interoperability, John Halamka (Chair of HITSP and CIO for Harvard Medical School and Beth Israel Deaconess) believes that "we can achieve a substantial improvement in care quality and coordination by implementing the systems available now." He posits that the definition of healthcare technology interoperability that is "good enough" includes:
- "Support for medication interoperability such as e-prescribing linking providers, payers, and pharmacies
- Support for laboratory and radiology interoperability such as orders and results integration among providers, hospitals and commercial labs
- Support for seamless electronic interchange between providers and payers for administrative data flows.
Transition into product, and incentive systems for EHR adoption, has been accelerated through certifications including interoperability standards. Mark Leavitt, Chair of the Certification Commission for Healthcare Technology (CCHIT), recently reported on the existing certification programs, which started with an ambulatory EHR certification program launched in 2006.

Take time to parse the following from Mark Leavitt: "That there are no good products is absolutely not the problem".
Secretary Mike Leavitt argues that that Obama's Recovery and Reinvestment Plan should require that investments in health IT systems be certified interoperable. This "could spur a critical mass of the nation's doctors to finally enter the information age... If we're going to build a 21st-century health infrastructure, we need to do it strategically, continuing the careful work on harmonized standards that will create one nationwide, interoperable system. That's the only way to make an investment in health IT produce value for providers and patients and improve the quality of health care overall."
Not everyone is convinced that these investments will pay off. David Kibbe (Senior Advisor to the American Academy of Family Physicians) and Brian Klepper argue that "the easy solution would be to spend most of the health IT funds on EHRs. The EHR industry has made it easy by establishing a mechanism to 'certify' EHR products if they incorporate certain features and functions." Kibbe and Klepper contend that EHRs are expensive, disruptive to implement, with no clear patient safety benefits and are not yet interoperable. "These barriers to adoption are well documented; they form the wall that has kept physician EHR adoption overall to less than 25 percent in this country. Even if a hefty federal subsidy reduced the exorbitant cost of the EHRs, many practices would suffer severe negative business impacts, and primary care access could temporarily be reduced on a national scale."
In the meantime, some healthcare organizations are waiting on the sidelines for the federal Recovery and Reinvestment Plan to be enacted before making new health IT investments.
Link here for more on the "Good Enough" debate in Healthcare Technology.
Tuesday, December 16, 2008
Value Cases: AHIC's New Artifact
So what exactly is a Value Case? Laura Miller, interim Executive Director for AHIC, discussed Value Cases with the National Committee of Vital and Health Statistics on November 18.
A Value Case "describes an opportunity for information exchange within the context of an interoperability roadmap illustrating specific scenarios for interoperability (similar to a use case) and demonstrates a case for action based technical, business, and societal risk adjusted value. Specifically, a Value Case presents the costs, value, and risks of implementing the specific scenario and describes potential measures of actual impact on improving care. Once recognized, it commits the submitting organization to fund and execute actions necessary to implement the case."
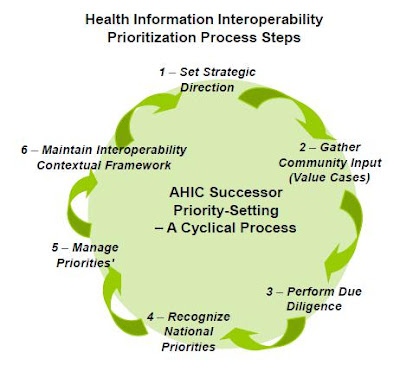 AHIC prioritization will be based on an overall interoperability strategy maintained byAHIC. A call for Value Cases from the healthcare community will begin in January 2009. Decisions on national priorities for this first round will be made in September 2009 with recommendations from expert committees (committees such as "Genomics, Chronic Disease Management or Clinical Research").
AHIC prioritization will be based on an overall interoperability strategy maintained byAHIC. A call for Value Cases from the healthcare community will begin in January 2009. Decisions on national priorities for this first round will be made in September 2009 with recommendations from expert committees (committees such as "Genomics, Chronic Disease Management or Clinical Research").HITSP and CCHIT will continue their roles in standards harmonization, standards development and certification, with HITSP transitioning to work on Value Cases in 2010.
This can't possibly work, can it? Pay for interoperability?
It willl work for the big players. The big Healthcare IT businesses will quickly grasp the opportunity to differentiate themselves through first-to-market leadership on carefully crafted Value Cases. Big payers will look for the opportunities to drive down cost related to the chronically ill and to the revenue cycle, among others. Innovation and cost reduction are important to healthcare nationally and will be well funded.
However, key national priorities related to population health management and needs of underserved populations don't necessarily have the financial backing to support syndication. AHIC recognizes that "Public Good Value Cases" may require "scholarship" funding. This is a crucial component to gain support across the broader healthcare community and may be the litmus test of the effectiveness of the new AHIC.
Tuesday, June 3, 2008
ONC roadmap - On the road to Abilene?
 The ONC synopsis focuses on 2 goals: Patient-focused Health Care and Population Health. ONC defines Patient-focused Health Care as "enabling the transformation to higher quality, more cost-efficient, patient-focused health care through electronic health information access and use by care providers, and by patients and their designees." Population Health "enables the appropriate, authorized, and timely access and use of electronic health information to benefit public health, biomedical research, quality improvement, and emergency preparedness." Themes of privacy and security, interoperability, adoption, and collaborative governance apply to each of these goals.
The ONC synopsis focuses on 2 goals: Patient-focused Health Care and Population Health. ONC defines Patient-focused Health Care as "enabling the transformation to higher quality, more cost-efficient, patient-focused health care through electronic health information access and use by care providers, and by patients and their designees." Population Health "enables the appropriate, authorized, and timely access and use of electronic health information to benefit public health, biomedical research, quality improvement, and emergency preparedness." Themes of privacy and security, interoperability, adoption, and collaborative governance apply to each of these goals. Critical mass in the use of CPR's combined with exchange of health information between providers and access to information by patients will be facilitated by the Nationwide Health Information Network.
Critical mass in the use of CPR's combined with exchange of health information between providers and access to information by patients will be facilitated by the Nationwide Health Information Network.ONC defined the criteria for success as:
- Health IT becomes common and expected in health care delivery nationwide for all communities, including those caring for underserved or disadvantaged populations;
- Your health information is available to you and those caring for you so that you receive safe, high quality, and efficient care;
- You will be able to use information to better determine what choices are right for you with respect to your health and care; and
- You trust your health information can be used, in a secure environment, without compromising your privacy, to assess and improve the health in your community, measure and make available the quality of care being provided, and support advances in medical knowledge through research.
There is solid momentum and engagement by HHS, healthcare providers, and healthcare IT companies. As an example of the energy level, CCHIT just reported that they had over twice as many volunteers as available roles in unpaid positions. There's clear value to patients and public health if these goals can be achieved.
 Certification Commission for Healthcare Information Technology (CCHIT) chair Mark Leavitt has talked about the critical need to address the mis-aligned costs and benefits in the health system. Leavitt positions CCHIT as the enabler to a more virtuous cycle. The critical ingredient still missing in this equation is provider incentives of sufficient substance to close this loop. Whether this is the Road to Abilene or not, depends on whether providers can buy in at a reasonable sustainable cost.
Certification Commission for Healthcare Information Technology (CCHIT) chair Mark Leavitt has talked about the critical need to address the mis-aligned costs and benefits in the health system. Leavitt positions CCHIT as the enabler to a more virtuous cycle. The critical ingredient still missing in this equation is provider incentives of sufficient substance to close this loop. Whether this is the Road to Abilene or not, depends on whether providers can buy in at a reasonable sustainable cost.
Monday, June 2, 2008
HITSP keeps on rolling

These specifications and definitions include:
Medication Dispensing Status provides a medication prescriber the dispensing status of an ordered prescription (dispensed, partially dispensed, not dispensed).Dr. Halamka announced he will also be presenting a technical note on Document Reliable Interchange to support a secure communication of a clinical document over a network.
Medication Orders defines the transactions between prescribers (who write prescriptions) and dispensers (who fill prescriptions)
Medication Formulary and Benefits Information performs two tasks: 1) performs eligibility check for a specific patient's pharmacy benefits and 2) obtains the medication formulary and benefit information.
Patient Generic Health Plan Eligibility Verification provides the status of a health plan covering the individual, along with details regarding patient liability for deductible, co-pay and co-insurance amounts for a defined base set of generic benefits or services. The base set of benefits includes coverage status and patient liability for medical, chiropractic, dental, hospital inpatient, hospital outpatient, emergency, professional physician office visit, pharmacy and vision services that are included in the patient's generic health plan benefit.









